Traumatic brain injuries, more commonly referred to as TBIs, are diagnosed using various methods – and sometimes diagnostic equipment is not necessary. How a TBI is diagnosed depends on the injury that caused it, the severity of symptoms, and the provider’s expertise in the area.
While most TBIs are diagnosed as “mild,” that does not mean they are not serious. A person with even a mild TBI needs to rest and make sure they avoid any future injuries too soon, or they could suffer a more serious condition that is often fatal. Also, even if someone feels fine, if they have suffered a serious injury involving their head, they should seek treatment. A physician may be able to diagnose a TBI even when a person is not experiencing serious symptoms, and knowing what to do to avoid any further damage is critical.
Assessment Tools Are a Common Method for Diagnosing a Traumatic Brain Injury
Typically, the initial assessment a physician will use is known as the Acute Concussion Evaluation (ACE). The U.S. Centers for Disease Control and Prevention created this tool for medical providers to quickly diagnose a TBI. It helps assess a person suspected of a mild TBI, such as a concussion.
The ACE process involves:
- Collecting information about the injury. The physician will first ask about the injury, how and where it occurred, and any symptoms that appeared immediately afterward.
- Identifying a loss of consciousness. Providers will ask if the patient lost consciousness. However, a person can still have a TBI without losing consciousness, so do not assume that you or a loved one is safe just because you didn’t.
- Asking what symptoms the patient experienced immediately after and if they worsened. Sometimes, a person does not seek treatment until symptoms begin. At this point, the physician will want to know what symptoms were present immediately following the incident, and then whether they got worse progressively, new symptoms arrived, and if any have gone away or lessened.
- Discussing the risk factors with the patient. The physician will also discuss risk factors that put them as being more likely to have a TBI than someone else. For example, if the injury occurred during a football game, the physician would consider that a high risk for a TBI.
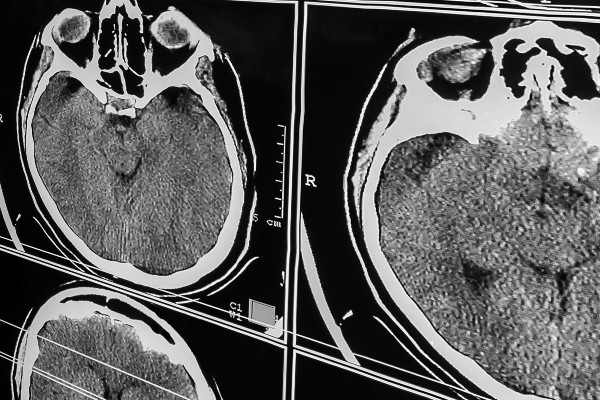
Using Diagnostic Scans to Determine the Presence of a TBI and Its Severity
Sometimes, a medical professional will need more than a quick assessment tool. When this occurs, they turn to diagnostic imaging. Brain scans not only help determine if a TBI exists, but can help them identify the severity of that TBI and possible treatment – especially if one is so severe that the patient requires surgery. Usually, a physician will only find a diagnostic scan necessary if they feel the patient’s symptoms are worrisome, the injury is more severe, or the patient was involved in a serious accident and they want to rule out a major TBI.
The most used scans include:
- Computed Tomography (CT) Scans – CT scans are the most used scan to assess whether a patient has a TBI or not. If the patient is suspected to have a moderate to severe TBI, the physician will use a CT scan to rule out any bleeding in the brain, contusions, swelling, and fractures. Usually, a CT is used more in an emergency room than after a visit with a neurologist, only because they are quick, easy to access, and still provide an accurate diagnosis for more serious head traumas.
- Magnetic Resonance Imaging (MRI) – After an initial assessment, the physician may feel more comfortable using an MRI to rule out serious head trauma. Sometimes an MRI offers a more detailed look, and it can pick up those subtle injuries that a CT could overlook.
- Diffusion Tensor Imaging (DTI) – This newer type of neuroimaging reviews the tracts of white matter in the brain and can look for damage.
- FLAIR – This looks for smaller areas of damage that an MRI and CT cannot pick up. This includes looking for minute instances of bleeding in the brain that is still serious, but not heavy enough to show up on a typical scan.
Conducting Neuropsychological Tests
When a TBI is too mild to show up on an MRI or CT, a physician may prefer to use neurological or neuropsychological tests. These are conducted by a neurologist or neuropsychologist. These tests look at overall brain function, examine a patient’s symptoms to see if they are similar to those associated with brain trauma, and often combine the use of diagnostic imaging with these examinations to determine if a patient is likely to have suffered a mild TBI.
Comparing Baseline Images in Athletes
For athletes, most organizations are now requiring a baseline diagnostic scan. Therefore, they will do a CT or MRI of their team member’s brain, and then compare it to a post-injury one to see if there are any changes. If they find changes, that may indicate a TBI occurred or they have recovered from a TBI recently. These baselines are critical in professional sports where the risk for serious brain injury occurs, such as football, hockey, and wrestling.
Did You or a Loved One Suffer a TBI Due to Someone’s Negligence? You Have Rights
If you or a loved one suffered a TBI due to someone’s negligent acts, you may be entitled to compensation. To explore your rights and to see if you have a case, contact our aggressive legal team at Brett McCandlis Brown & Connor, PLLC, today. We have helped countless victims and their loved ones receive full compensation for their brain injuries, including future costs that are often associated with these devastating incidents.
To get started, schedule a free case evaluation. We will sit down and discuss the circumstances of your accident and see if you have a valid brain injury claim – and you do not pay our team unless we recover compensation in your case.


